Patella Tendonitis
Patella Tendonitis or “Jumper’s Knee” occurs usually in sportsmen. It causes pain at the lower end of the knee cap, where the patella tendon is attached. The cause of the pain is usually due to over activity or secondary to local irritation and degeneration of the tendon by a bone spike on the lower end of the kneecap or patella.
Treatment is usually by rest and physiotherapy treatment. Occasionally steroid injection or keyhole surgery maybe required. Surgery involves removing any bone spikes from the patella and stimulating healing tissue in the tendon.
Rarely weakness of the inflamed tendon may result in a rupture.
Quadriceps Tendonitis Sinding Larrson Disease
Similar to patella tendonitis but much rarer. Occurs at the upper part of the patella. Physiotherapy and injections are the usual remedies. Surgery rarely necessary.
 Osgood Schlatters Disease.
Osgood Schlatters Disease.
This condition usually occurs in adolescent children. It is related to sport and is cause by the pull of the patella tendon on the front of the upper shin bone. The patella tendon is attached to a separate bone on the front of the shin bone. These bones eventually join together at the end of full growth. Whilst growing this bone can be distorted by excessive pull of the patella tendon. The result is that this bony attachment of the tendon becomes larger forming a painful lump on the upper front part of the shin bone.
The usual treatment is rest and the end result is a painless lump at the upper shin bone.
Occasionally patients may have pain that persists or recurs in the early twenties. This is usually due to small pieces of bone (ossicles) at the site of attachment of the patella tendon. These can be removed to relieve symptoms.
Reflex Sympathetic Dystrophy (RSD)
RSD involves a group of symptoms which are the result of the nerves supplying the knee being hypersensitive. Patients experience pain out of proportion to the original injury. The injury may include operations: keyhole or open surgery, direct blows to the front of the knee, minor twists or knocks. The knee may be stiff and swollen. In most cases the front of the knee is very sensitive such that clothes: trousers or tights may be painful to wear. Bed clothes may also be uncomfortable on the front of the knee. In severe cases the skin around the knee may undergo colour changes such as red flushing, purple or white.
Treatment involves reassurance of no serious knee injury despite severe pain. MRIs are normal. Physiotherapy, massage, friction rubs and pain control measures are the keys to successful treatment. Surgery should not be undertaken and patient’s inability to go through the pain barrier may lead to chronic pain and disability for the patient.
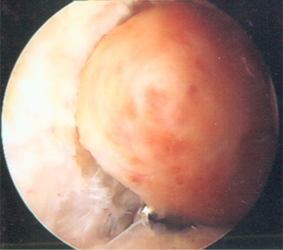 Pigmented Villonodular Synovitis (PVNS)
Pigmented Villonodular Synovitis (PVNS)
This is a rare condition that affects the knee and presents with swelling, stiffness and pain in the knee. The lining of the knee joint or synovium begins to thicken and form grape like and finger shaped swellings. The synovium also changes colour to a brown chocolate colour. These swellings produce more fluid and so the knee becomes markedly swollen.
The condition behaves like a benign tumour in that it can recur after the synovium is removed and it may also spread outside the knee joint.
PVNS is treated by keyhole and open surgery to remove the synovium. Radiotherapy to the knee joint is occasionally necessary and long term follow up to ensure the disease is kept under control. Failure to control the disease may result in osteoarthritis and therefore knee replacement surgery.
Plicae Syndrome
In the knee joint there are folds of tissue called plicae. There are three well described plicae in the knee, the one on the inner side of the knee being the one that may cause pain in the knee, These folds may be injured and become inflamed and scarred. They may also become trapped or pinched between the knee cap and thigh bone. Treatment includes, rest painkillers local physiotherapy treatments and on rare occasions surgery.
This is a controversial topic as some experts believe that plicae are not responsible for knee pain.
Ganglia in the Knee Joint.
Ganglia are swellings which have a thin tissue wall and are filled with thick clear fluid. They are commonly associated with tendons around the wrist. Rarely they can occur as cysts in the knee joint around the ligaments and fat pad of the knee joint. These cysts are usually seen on MRI scans as coincidental findings. They may be a source of knee pain and can be removed by keyhole surgery.
 Bone Bruises
Bone Bruises
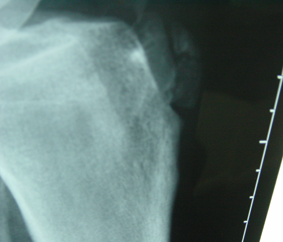
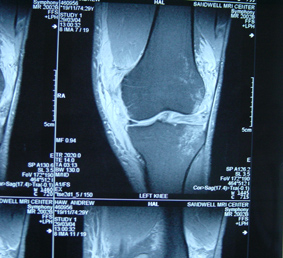
This injury can only be diagnosed by MRI scans and therefore have only been known to surgeons since the wide availability of MRI. Bone bruises can occur at the same time as ligament injuries when the knee has been twisted. They can occur as flare ups of osteoarthritis or after keyhole surgery for treatment of osteoarthritis
Avascular Necrosis (AVN) of the knee joint:
.JPG) This condition occurs rarely as a spontaneous event, but may occur in patients who are on long term steroids such as transplant patients. In the spontaneous variety the condition usually affects middle aged patients with some degeneration already in the knee. The blood supply to a small area on the end of the femur or thigh bone becomes blocked, the bone dies and the overlying cartilage breaks up. This can produce acute pain in the knee. The diagnosis is made by an MRI Scan. Sometimes the blood supply is restored and the bone can heal and scar tissue formed where the cartilage has been damaged. The pain then usually improves. Keyhole surgery, cartilage and bone grafting may occasionally be used but the common treatment is part or total knee replacement depending on the extent of the damage.
This condition occurs rarely as a spontaneous event, but may occur in patients who are on long term steroids such as transplant patients. In the spontaneous variety the condition usually affects middle aged patients with some degeneration already in the knee. The blood supply to a small area on the end of the femur or thigh bone becomes blocked, the bone dies and the overlying cartilage breaks up. This can produce acute pain in the knee. The diagnosis is made by an MRI Scan. Sometimes the blood supply is restored and the bone can heal and scar tissue formed where the cartilage has been damaged. The pain then usually improves. Keyhole surgery, cartilage and bone grafting may occasionally be used but the common treatment is part or total knee replacement depending on the extent of the damage.
Fat Pad Syndrome (Hoffa’s Syndrome):
There is a fat pad inside the knee joint that lies behind the patella tendon and in front of the femur. The fad pad can become trapped behind the knee cap and be pinched, bruised and swollen. This is thought to produce anterior knee pain in some patients. This is a controversial condition as is the plicae syndrome, as these structures would normally be in contact with the knee cap and the femur in normal knee movements.
Discoid Meniscus
The normal meniscus is crescent shaped structure, in development in the womb it starts out as a disc or plate shape and gradually is sculptured to a crescent shape by birth. If this change of shape does not occur the meniscus will always be plate shaped. This usually occurs in the outer meniscus. The discoid meniscus may not cause any symptoms at all. It is though more prone to tears. In toddlers or children it may present with a knee that clunks because the meniscus is also very loose in the knee. The knee may also be painful and the child may walk with a slightly bent knee, occasionally the knee may lock.
Treatment is usually surgery to trim the meniscus to a normal shape and to secure the loose meniscus.
Bursitis
A bursa is a normal structure in the body. They are flattened thin walled sacks of tissue with a thin film of fluid inside. They help to cushion bony prominences like the knee cap the front of the shin bone and the elbow. They also lie between muscles and tendons and allow smooth movement of muscles and tendons over each other.
Around the knee joint there are fourteen bursae. The bursae can become inflamed and swollen and therefore cause pain. The common bursae to be affected are at the front of the knee so called “Housemaids Knee” or “Preachers Knee” as a consequence of prolonged kneeling. The condition therefore presents with a localised ball shaped swelling at the front of the knee, the swelling maybe red and swollen.
Treatment includes rest, avoidance of pressure on the swelling, using antinflammatories or indeed antibiotics if the bursa becomes infected. Surgery is rarely indicated unless the selling becomes infected.
Nerve Neuromas
During surgery when the skin has to be cut nerves that run just under the skin are inevitably cut. Most nerves will re-grow and sensation will be restored. However some cut nerves do not heal properly and form a ball of nerve tissue on the end of the cut nerve. This ‘ball’ of nerve tissue or ‘neuroma’ can then be very sensitive under the skin and be the source of quite significant localised sharp pain when the skin over the neuroma is touched. Treatment includes injection with local anaesthetic and steroid. Excision of the neuroma maybe considered but the neuroma can recur.
Non Specific Synovitis – Gout, Pseudo gout
The knee joint can become swollen for many reasons in the absence of any injury. The lining of the joint or synovium normally produces and reabsorbs the fluid in the knee. This fluid is normally just a film of fluid to allow optimum lubrication of the joint. The synovium is very sensitive to irritation from particles such as crystals, articular cartilage, micro organisms etc.. and the joint will swell under these circumstances; so called Synovitis and effusion. The swollen knee will feel stiff and tight with a dull ache, restricted movement and the sensation of giving way of the knee.
Non specific Synovitis when the cause is unknown (probably secondary to a viral infection) is usually self limiting and will improve with time rest and antinflammatories. Synovitis secondary to gout crystals again will improve with rest and antinflammatories, and will usually require long term treatment to prevent recurrence.