 What is Instability?
What is Instability? The shoulder is the most mobile joint in the human body. The design of the two surfaces that form the joint (ball & socket) is less restrained than any other joint, to allow for the increased mobility. However, this reduction in restraints means the shoulder joint surfaces are prone to move apart. This abnormal movement of the two joint surfaces in relation to each other is called instability.
What is a shoulder dislocation?
A dislocation is a complete separation of the two joint surfaces (ball & socket) of the shoulder joint. Most of the time this occurs following an injury and is called 'Traumatic dislocation'. However, it may happen without an injury and is called 'Atraumatic instability or dislocation'. With repeated (sometimes called recurrent) dislocations, the force needed to dislocate the shoulder becomes less and the dislocation may even happen during sleep.
Do I have to dislocate my shoulder to have instability?
No. Instability may manifest itself as a shoulder subluxation (when the two surfaces of the joint separate partially and get back in position without help) or even just pain. Instability manifesting itself as pain is common in people in their teens, twenties & early thirties particularly if they do overhead sports such as tennis and swimming (Sports injuries) .
Are there any other joints around the shoulder that can be unstable?
Yes instability can affect the outer end of the collarbone discussed under AC Joint-Collar bone or the inner end of the collarbone discussed under AC Joint-Collar bone .
Which direction does the shoulder dislocate?
Anterior shoulder dislocation, when the ball moves forward in relation to the socket, is by far the most common way to dislocate the shoulder, occurring 95% of the time. However, Posterior shoulder dislocation (Sports injuries) or even Inferior shoulder dislocation is possible.
What happens when a shoulder dislocates?
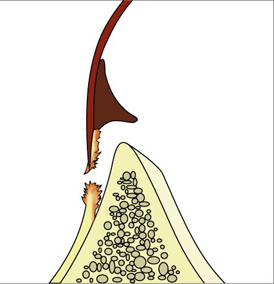 In younger people (under 40 years), muscle tendons are stronger than ligaments. As the ball of the shoulder joint moves forward, the ligaments attached to the shoulder socket are torn. This is called a labral tear or Bankart lesion.
In younger people (under 40 years), muscle tendons are stronger than ligaments. As the ball of the shoulder joint moves forward, the ligaments attached to the shoulder socket are torn. This is called a labral tear or Bankart lesion.
In older people (over 40 years), muscle tendons are weaker than ligaments. As the ball of the shoulder joint moves forward, the muscle tendons (rotator cuff) attached to the shoulder ball are torn. This is called a Rotator cuff tear .
What is the best treatment for a shoulder dislocation?
A dislocated shoulder has to be put back in joint as urgently as possible. This is best done in the accident & emergency department under sedation. Rarely, this requires a general anaesthetic. The shoulder is then rested in sling for 3-4 weeks followed by physiotherapy to regain movement and strength.
If the shoulder dislocation is not put back or as occasionally happens is missed, it becomes progressively more difficult to put back in joint. This may require an open operation. The longer the period the shoulder is dislocated (called chronic dislocation), the more complex the surgery required to put it back is.
What happens to the torn ligaments or muscle tendons?
Torn ligaments heal, but may not heal in the right position on the shoulder socket or may be stretched. This may lead to repeated dislocations in the future. This is more likely to happen the younger you are and the more active you are.
Torn muscle tendons do not heal and may require further treatment, as discussed under Impingement & rotator cuff .
What can be done to stop the shoulder from dislocating again?
The position the shoulder is rested in, in the sling after the dislocation may be important in allowing the ligaments to heal in the right position on the socket. Physiotherapy improves awareness of shoulder position and strength and may help stop further dislocations.
Very occasionally, a high level young athlete may need surgery to stop the shoulder from dislocating again.
What happens if the shoulder dislocates again?
Your doctor will examine you and if necessary organise for you to have an MR/Arthrogram, to assess whether the ligament tear has not healed or healed in the wrong position.
It is very likely that the shoulder would continue to dislocate with less severe injuries or even doing normal day to day things if it has dislocated more that once. Therefore, surgery will have to be considered.
What surgery do I need to stop the dislocations?
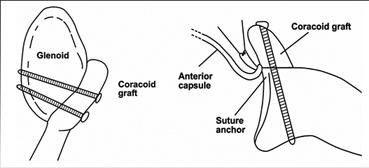
The principle of surgery for shoulder dislocation is to repair the torn ligaments (labral tear or Bankart lesion) in the correct position on the socket of the shoulder joint.
Most of the time, this is possible with a keyhole operation rather than an open operation. An open operation may be required after numerous dislocations, where the repeated dislocations have worn off part of the socket bone or the ligaments have been stretched too far.
If the keyhole operation is possible (over 85% of the time), it has the advantage of less pain, smaller scar and no scarring in the surrounding muscle tendons.
What does an operation mean for me?
The operation is done under a general anaesthetic and means one night in hospital. You will need to wear a sling for 3-4 weeks after the operation. You will not be able to drive for 6 weeks. If you have a less physical job, you will be able to get back to work when you can drive. For a more physical job, you may be off work for 2-3 months.
Return to sport will depend on the type of sport. Swimming breaststroke is allowed when the sling is off. Overhead sports are allowed at 3 months and contact sports at 4 months.
What if my shoulder instability happened without injury?
Some people have a lax shoulder, which means the lining of the joint (capsule) is thin and of a bigger volume than the average, people are born with that. Lax shoulders function as normal, but can become unstable more easily than normal shoulder. Instability can happen after simple actions such as throwing a ball. This type of instability is called atraumatic instability or multidirectional instability.
What is different about atraumatic 'multidirectional' instability?
The problem is normally a stretching of the originally lax shoulder capsule, which allows abnormal movement of the shoulder ball. The abnormal movement may, sometimes, occur in different directions (anterior, posterior or inferior) in the same shoulder, hence the name multidirectional instability. This is different from traumatic instability that happens in one direction, usually anterior, as mentioned above.
What does atraumatic 'multidirectional' instability feel like?
This problem usually occurs in teenagers and people in their twenties. How bad the problem is depends on the degree of stretching of the capsule. A minor stretch may just cause episodes of pain when playing overhead sport. With further stretching the pain may follow any activity or the shoulder may feel like it is partially coming out of joint (subluxation). Shooting pains down the arm can occur. If the joint capsule is very stretched, dislocations can happen and sometimes in different directions at different times.
How do I know if I have atraumatic 'multidirectional' instability?
Your doctor will examine you and if there is any doubt, will organise for you to have an MR/Arthrogram scan to make sure. The scan is usually normal in this condition.
How can atraumatic instability be treated?
In 90% on the time, this can be treated with physiotherapy alone. Physiotherapy to increase your sense of awareness of the shoulder position and build up the muscles around the shoulder joint and shoulder blade will normally return the lax shoulder to a stable condition.
What if physiotherapy does not work?
Physiotherapy is a prolonged process for this condition, taking up to one year to regain control of the shoulder. Surgery is only helpful to assist physiotherapy and is not successful on its own.
The aim of surgery is to reduce the volume of the lining of the shoulder joint (capsule). The way this is done depends on how stretched the capsule is. This can be achieved by radiofrequency capsular shrinkage or arthroscopic capsular shift, if the stretching is moderate. Both these operations are keyhole operations. Severe capsular stretching can be treated with an open capsular shift operation.
What these operations mean for you will depend on the severity of the problem with a period in a sling that varies from 1 week with radiofrequency capsular shrinkage to 6 weeks with a capsular shift operation. Return to driving is normally possible 2 weeks after the sling comes off and return to a less physical job is possible then.
Back to top